Dec 24 2012
Leonidas Hill recently made history at Mattel Children's Hospital UCLA, when the 5-year-old became the first pediatric patient in the western United States to undergo transoral robotic surgery (TORS) - a minimally invasive surgery performed with the help of a robot - to repair a rare congenital condition known as a laryngeal cleft.
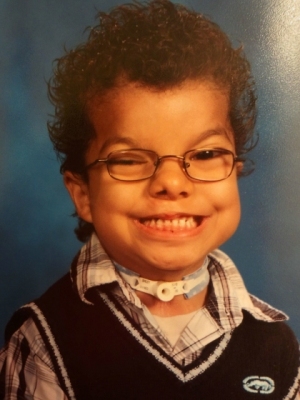 Leonidas Hill
Leonidas Hill
Mattel Children's Hospital UCLA is one of only a handful of medical centers in the country offering this type of surgery, which is rarely done on pediatric patients. The technology allows surgeons to perform the operation through the mouth of the patient, rather than in the traditional manner, which requires external incisions and the splitting of the patient's voice box.
Hill was born with both a laryngeal cleft and a cleft lip/palate, defects that occur during embryonic development. The cleft is an extremely rare airway defect in the laryngo-tracheal wall, which results in an abnormal opening between the larynx and the esophagus. This allows food to get into the airways and even the lungs.
Hill's cleft, which was classified as Type 3 (Type 4 is the most severe), extended beyond his voice box and into his trachea, leading to tracheomalacia, a condition that occurs in newborns in which the cartilage of the trachea, or windpipe, has not developed properly. Because of this, the trachea walls, instead of being rigid, are floppy and collapse, resulting in breathing difficulties.
Hill's breathing difficulties began soon after birth, and he underwent a tracheotomy-tube placement as an infant to help with his airway issues. Due to his chronic aspirating, he also had a gastrostomy tube placed in his stomach to minimize respiratory infections such as pneumonia and bronchitis.
Dr. Nina Shapiro, director of pediatric otolaryngology at Mattel Children's Hospital UCLA and an associate professor of surgery at the David Geffen School of Medicine at UCLA, diagnosed Hill's cleft and recommended him for the TORS procedure.
"The benefit of the surgical robot is that it gives more access to the pediatric airway using minimally invasive techniques," she said. "For Leonidas, this surgery repaired his cleft, which will greatly improve his airway issues and put him in a better position for removing the tracheotomy tube."
The Da Vinci robotic surgical system, the state-of-the-art technology used at UCLA, is a minimally invasive procedure in which a surgical robot, under the full control of a specially trained physician, operates with a three-dimensional, high-definition video camera and robotic arms.
These miniature "arms" can navigate through the small, tight and delicate areas of the mouth without the need for external incisions. A retraction system allows the surgeon to see the entire surgical area at once. While working from an operating console, every movement of the surgeon's wrists and fingers are transformed into movement of the surgical instruments.
Dr. Abie Mendelsohn, an assistant professor of surgery at UCLA, developed the TORS program at the UCLA Department of Head and Neck Surgery. Mendelsohn operated on Hill and repaired the cleft in the back of his larynx.
After examining the cleft, Mendelsohn used a special carbon-dioxide laser-fiber adapter for the robot to destroy the cleft's inner lining, which allowed for wound-healing of the cleft. Following the laser procedure, Mendelsohn used the robot to transorally place sutures within the larynx and trachea to hold the two ends of the cleft together.
"This type of laryngeal cleft repair traditionally requires open surgery, which entails a very large neck incision, splitting the voice box, and direct suturing of the cleft," Mendelsohn said. "This approach is highly invasive, has a prolonged surgical time and requires an extensive healing period. Using the TORS method, our approach did not require any skin incisions, there was direct access to the closure site, no visible scars and a faster healing time, so Leonidas was able to go home the next day. The TORS procedure shortens hospital stays for patients, and they can get back to their lives faster and with fewer limitations."
Hill made a speedy recovery and was back at school within days. His prognosis is good, and Shapiro said that the next step will be to perform additional tests, with the hope of removing Hill's tracheotomy tube.
"The ultimate goal is to remove the tracheotomy and gastrostomy tubes so that Leonidas can swallow liquids and solids by mouth," she said. "This surgery will help him breathe easier and work toward eating and drinking on his own."
With continuing pediatric adaptations made to the robotic surgical instruments, physicians and surgeons at UCLA will continue to search for appropriate pediatric candidates for robotic surgical procedures.
"The initial robotic surgical instruments had an outer diameter of 8 millimeters, which has now been improved to 5 millimeters," Mendelsohn said. "Additionally, the initial robotic endoscope had an outer diameter of 15 millimeters, which has now been improved to 8.5 millimeters. These improvements have led to our ability to fit the instrumentation successfully through the mouth of a pediatric patient. In our eyes, this experience was successful, and we believe that with selected pediatric patients, robotics will have a continued use at the Mattel Children's Hospital UCLA."