Mar 20 2020
Scientists at the University of Massachusetts Amherst (UMass) have developed a mobile surveillance device called FluSense that is powered by machine learning. The device can detect the size of the crowd and coughing in real time and subsequently inspect the data to directly track influenza and flu-like disease trends.
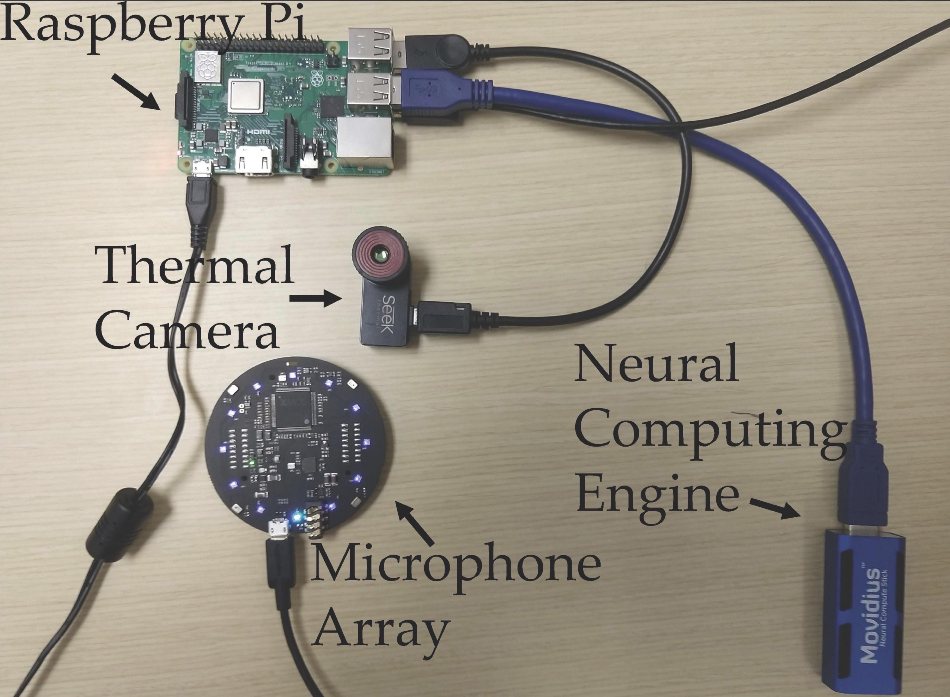 The FluSense device houses these components. Image Credit: University of Massachusetts Amherst.
The FluSense device houses these components. Image Credit: University of Massachusetts Amherst.
According to the developers of FluSense, the revolutionary computing platform, projected for use in healthcare waiting rooms, hospitals, and larger public spaces, is likely to contribute to the increase in the collection of health surveillance tools used for predicting seasonal flu and other similar viral respiratory outbreaks such as SARS and the COVID-19.
By directly conveying the public health response, such models can act as lifesavers during the time of flu epidemics. Data sources like these can help ascertain the timing for potential travel restrictions, flu vaccine campaigns, and the distribution of medical supplies, etc.
This may allow us to predict flu trends in a much more accurate manner.
Tauhidur Rahman, Study Co-Author and Assistant Professor, University of Massachusetts Amherst
Also, Rahman advises the study’s lead author and PhD student, Forsad Al Hossain.
The researchers’ results on FluSense study were recently published in the journal—Proceedings of the Association for Computing Machinery on Interactive, Mobile, Wearable and Ubiquitous Technologies.
In an effort to give their innovation a real-world testing, the inventors of FluSense teamed up with Dr George Corey, executive director of the University Health Services; Nicholas Reich, biostatistician and director of the UMass-based CDC Influenza Forecasting Center of Excellence; and Andrew Lover, an epidemiologist, assistant professor in the School of Public Health and Health Sciences, and a vector-borne disease expert.
The new FluSense platform has the ability to process thermal imaging data and a low-priced microphone array, with a neural computing engine and Raspberry Pi. It does not store any personally identifiable data, like distinguishing images or speech data.
In Rahman’s Mosaic Lab, where the sensors are created by computer researchers to monitor the health and behavior of humans, the scientists initially developed a laboratory-based cough model. Then by training the deep neural network classifier, they drew bounding boxes on thermal images that represented people and subsequently counted them.
“Our main goal was to build predictive models at the population level, not the individual level,” added Rahman.
The researchers positioned the FluSense devices, which were enclosed in a rectangular box resembling the size of a huge dictionary, in four healthcare waiting rooms at the University Health Services clinic in UMass Amherst.
From the period of December 2018 to July 2019, the new FluSense platform was able to gather and examine over 21 million non-speech audio samples and 350,000 thermal images from the public waiting areas.
The scientists discovered that the FluSense device has the ability to precisely estimate the rates of day-to-day illnesses at the university clinic. Complementary and multiple sets of FluSense signals “strongly correlated” with lab-based testing for influenza and flu-like illnesses itself.
According to the research, “the early symptom-related information captured by FluSense could provide valuable additional and complementary information to current influenza prediction efforts,” like the FluSight Network, which happens to be a multidisciplinary consortium of flu forecasting teams. The Reich Lab at UMass Amherst is also a part of this consortium.
I’ve been interested in non-speech body sounds for a long time. I thought if we could capture coughing or sneezing sounds from public spaces where a lot of people naturally congregate, we could utilize this information as a new source of data for predicting epidemiologic trends.
Tauhidur Rahman, Study Co-Author and Assistant Professor, University of Massachusetts Amherst
According to Al Hossain, FluSense is an illustration of the power of integrating edge computing with artificial intelligence—the frontier-pushing trend that makes it possible to collect and analyze the data correctly at the data’s source.
“We are trying to bring machine-learning systems to the edge,” stated Al Hossain pointing to the small components integrated into the FluSense device. “All of the processing happens right here. These systems are becoming cheaper and more powerful.”
The subsequent step is to test the FluSense device in geographic locations and other public areas.
We have the initial validation that the coughing indeed has a correlation with influenza-related illness. Now we want to validate it beyond this specific hospital setting and show that we can generalize across locations.
Andrew Lover, Epidemiologist and Assistant Professor, School of Public Health and Health Sciences, University of Massachusetts Amherst