Nov 14 2018
Scientists at Worcester Polytechnic Institute (WPI) and Albany Medical College, together with corporate partners GE Global Research and Acoustic MedSystems Inc., have obtained a five-year, $3.5 million award from the National Institutes of Health (NIH) through the National Cancer Institutes’ (NCI) Academic-Industrial Partnership program, to continue the creation of a novel robotic system that has the ability to operate within an MRI scanner to deliver a minimally invasive probe into the brain to eliminate metastatic brain tumors using high-intensity therapeutic ultrasound through real-time guidance.
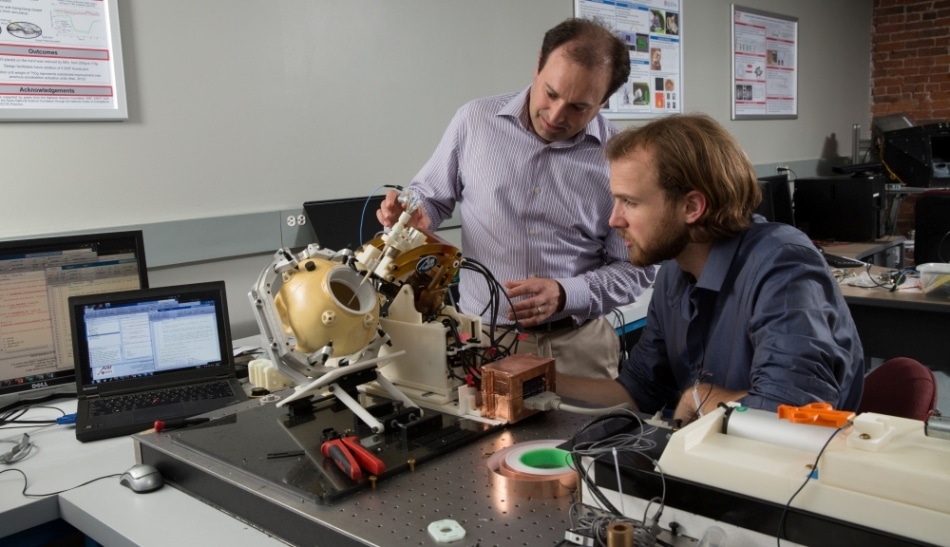 Mechanical engineering professor Gregory Fischer, left, and research scientist Christopher Nycz examine a prototype of the MRI-compatible robotic system for treating brain tumors developed in the first phase of the NIH-funded research program. (Image credit: Worcester Polytechnic Institute)
Mechanical engineering professor Gregory Fischer, left, and research scientist Christopher Nycz examine a prototype of the MRI-compatible robotic system for treating brain tumors developed in the first phase of the NIH-funded research program. (Image credit: Worcester Polytechnic Institute)
The grant is the second major NIH award for the development of the system and will allow the researchers to model the ultrasound ablation system’s behavior, execute thermal monitoring to offer real-time feedback on dose delivery, improve and validate the system’s effectiveness, and approve the readiness of the system for human clinical trials.
The team has been headed by principal investigators Gregory S. Fischer, PhD, associate professor of mechanical engineering and robotics engineering at WPI and director of the Automation and Interventional Medicine Laboratory, and Julie G. Pilitsis, MD, PhD, chair of the Department of Neuroscience and Experimental Therapeutics and professor of neurosurgery at Albany Medical College.
Fischer and Pilitsis will work in close collaboration with the two corporate partners. Acoustic MedSystems in Savoy, Ill., will design, construct, and verify the needle-based therapeutic ultrasound (NBTU) probe and offer the software to visualize and control it. GE Global Research Center in Niskayuna, N.Y., will execute thermal imaging capabilities to perform real-time monitoring of the ablation of tumor tissue, and will collaborate on incorporating the robotic system into its clinical MRI scanner.
Brain metastases—the most common type of brain tumors—occurs when primary cancers from other organs spread to the brain. Every year, nearly 170,000 new cases are diagnosed in North America. At present, chemotherapy, radiation, and surgery the only treatment options, which find limited success and can affect the unaffected brain tissue; moreover, surgery is feasible only if the tumors are in accessible locations.
The treatment strategy of the system being developed with the NIH award is different. The system is equipped with a thin, 2-mm-diameter probe that can be inserted into the brain via a small hole drilled in the skull and positioned within the tumor. Doctors will be in a position to deliver doses of high-intensity ultrasound energy lethal to tumors by tuning the probe’s orientation and power output, while minimizing damage to surrounding brain tissue. High-intensity ultrasound energy destroys tissue by heating it, known as thermal ablation, rendering it feasible to use an MRI scanner’s potential to detect thermal emissions to monitor the dose delivered to the tumor.