Reviewed by Lexie CornerMar 8 2024
A new study published in the journal JAMA Ophthalmology reveals that artificial intelligence (AI) technology can autonomously and reliably detect 100 % of severe cases of a condition that causes blindness in prematurely born infants.
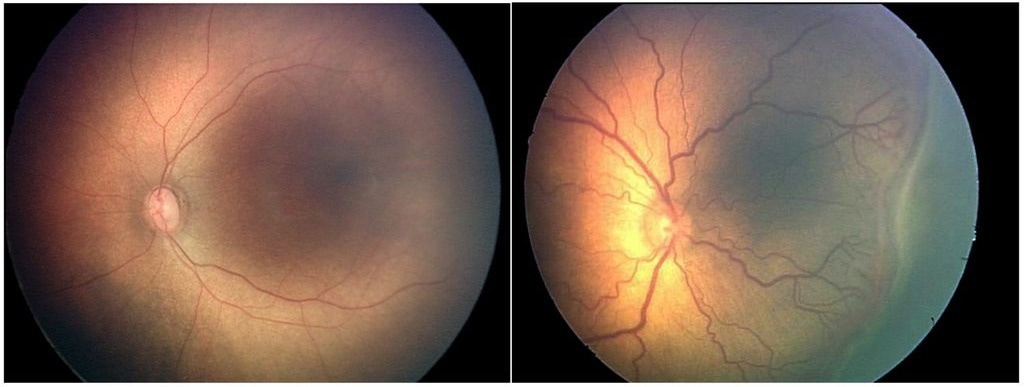 Retinopathy of prematurity. ROP can be diagnosed by examining the vessels of the retina at the back of the eyes. Here are two such images: one of a normal eye (left) and another of an eye with twisted and dilated retinal vessels, which indicates ROP. OHSU and Massachusetts General Hospital have developed an artificial intelligence-based algorithm that more accurately diagnosed ROP in images such as these than most of the eight expert physicians involved in the study. Image Credit: OHSU/Michael Chiang.
Retinopathy of prematurity. ROP can be diagnosed by examining the vessels of the retina at the back of the eyes. Here are two such images: one of a normal eye (left) and another of an eye with twisted and dilated retinal vessels, which indicates ROP. OHSU and Massachusetts General Hospital have developed an artificial intelligence-based algorithm that more accurately diagnosed ROP in images such as these than most of the eight expert physicians involved in the study. Image Credit: OHSU/Michael Chiang.
Conducted by researchers from Oregon Health & Science University (OHSU) and partners, the study highlights the AI’s remarkable accuracy in diagnosing this condition.
This technology has the potential to significantly enhance worldwide screening efforts and, ultimately, sight-saving treatments for retinopathy of prematurity (ROP). It is the same condition that caused musician Stevie Wonder to go blind.
ROP occurs when there is abnormal blood vessel growth near the retina, the light-sensitive tissue at the back of the eye. Each year, approximately 2 million babies are born prematurely, putting them at risk of developing ROP. However, in most instances, the disease is mild and resolves without the need for treatment.
Severe cases affect around 500 babies in the United States and approximately 50,000 babies worldwide, leading to blindness annually. In low- and middle-income countries, where there are not many ophthalmologists to examine and treat premature babies, more cases go untreated.
ROP is the leading cause of blindness in children in the U.S. and around the world and perhaps the most solvable problem among many in global efforts to reduce preventable blindness. Although we cannot fully prevent ROP, we can almost always prevent blindness from ROP.
J. Peter Campbell, MD, MPH., Study Corresponding Author and Associate Professor, Ophthalmology, School of Medicine and Casey Eye Institute, Oregon Health & Science University
Campbell added, “While there are doctors who are skilled in ROP treatment in many parts of the world, there simply aren’t enough to screen all of the babies who are at risk,” Campbell added. “This paper demonstrates that AI can effectively replace the physician for bedside screening and refer the most urgent cases to a physician for treatment.”
Tech to Expand Care
While at OHSU, Michael Chiang, MD, currently the director of the National Eye Institute at the National Institutes of Health, and his colleagues pioneered the development of the i-ROP Deep Learning system. This system employs an AI algorithm to detect anomalies in blood vessels in retinal images. Diagnosing ROP requires a manual review of these images by specially trained ophthalmologists.
Previous research by the team demonstrated that their AI technology could precisely diagnose ROP. It can be utilized effectively through telemedicine appointments, eliminating the need for conventional, in-person eye examinations.
This new study represents the first instance where independent AI screening for ROP has been proven effective in a real-life population. This means that the technology can correctly identify the condition without the need for an ophthalmologist and without preselecting photos to enhance data quality. While numerous AI algorithms succeed in regulated experiments, they frequently fail in practical settings due to differences between training data and actual usage settings.
The AI system in this study examined approximately 12,000 images of over 4,000 retinas of babies. These images were captured by nurses at neonatal intensive care units in hospitals in the United States and India.
Ophthalmologists reviewed the photos as part of telemedicine platforms in both countries. They found that approximately 1.2 % of the infants had severe forms of ROP, while around 5.8 % had more than mild cases. The AI technology correctly detected all severe cases and accurately sensed 80 % of the cases with more-than-mild ROP.
The i-ROP Deep Learning system was originally created by scientists from OHSU, the University of Illinois Chicago, Northeastern University, Massachusetts General Hospital, and the Imaging & Informatics in ROP (i-ROP) consortium. In 2020, the Food and Drug Administration (FDA) granted breakthrough status to the technology to advance its development.
In addition to his position at OHSU, Campbell serves as Siloam Vision’s chief executive officer, the company that licensed the technology. Siloam Vision is currently managing clinical trials to assess the safety and effectiveness of the AI system. The company has partnered with the nonprofit organization Orbis International to deploy the technology in low- and middle-income nations.
If the technology receives approval from regulatory organizations, ROP will become the second eye disease autonomously detected by AI. Currently, diabetic retinopathy, the leading cause of blindness in working-age adults affecting those with diabetes, can already be detected using three autonomous AI systems permitted for use in the United States.
This study received support from the National Eye Institute of the National Institutes of Health (grant numbers: R01 EY019474, R21 EY031883, R01 EY031331, and P30 EY010572), Research to Prevent Blindness (Career Development Award), the Eunice Kennedy Shriver National Institute Of Child Health & Human Development of the National Institutes of Health (grant number: R01 HD107494), the US Agency for International Development, the Seva Foundation, the Malcolm Marquis Innovation Fund, and the National Eye Institute’s intramural research program.
Journal Reference:
Coyner, S. A., et al. (2024) Multinational External Validation of Autonomous Retinopathy of Prematurity Screening. JAMA Ophthalmology. doi:10.1001/jamaophthalmol.2024.0045.