Predicted to become the second major cause of cancer-related fatalities in the US by 2030, pancreatic cancer has a grim prognosis, with almost 70% of patients facing mortality within the first year of diagnosis. Alarmingly, 40% of small pancreatic cancers evade detection on CT scans until they have progressed to an incurable stage.
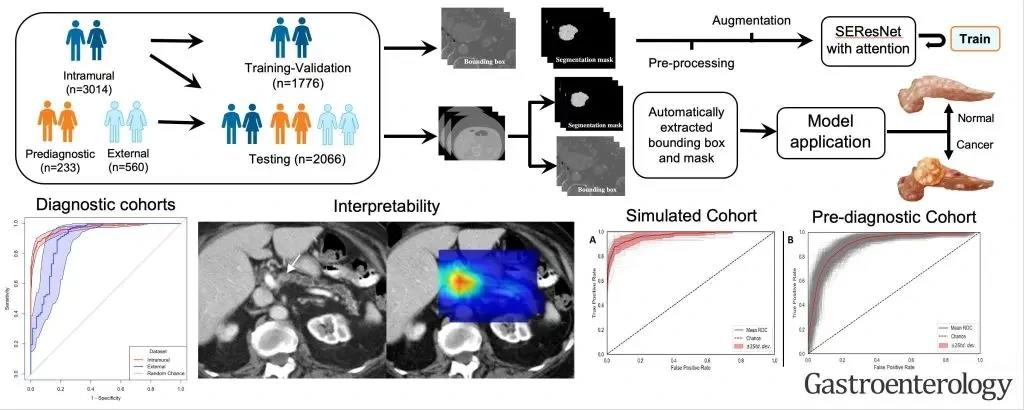
Image Credit: Mayo Clinic
This creates a critical "last-mile" barrier for early detection efforts where, in most patients — including those high-risk subjects undergoing active screening — imaging detects the cancer at a stage when a cure is unlikely. This makes imaging the final frontier in the quest for early cancer detection.
In a recent innovation, researchers from the Mayo Clinic Comprehensive Cancer Center built a flexible artificial intelligence (AI) model using the largest imaging dataset in the world. This model has the potential to automatically detect pancreatic cancer on standard CT scans when surgical intervention can still offer a cure.
This is where the study emerges as a beacon of hope. It addresses the last-mile challenge—detecting the cancer at a stage when the cancer is even beyond the scope of experts.
Ajit H. Goenka, Study Corresponding Author, Radiologist and Principal Investigator, Mayo Clinic
The group developed a highly accurate AI model, trained on the largest — more than 3,000 patients — and most diverse CT dataset for fully automated cancer detection, including small and otherwise difficult-to-detect tumors.
The study, which was published in the American Gastroenterological Association’s journal Gastroenterology, not only advances the team’s recent work on radiomics-based early detection models but also highlights Mayo Clinic’s position as a leader in AI healthcare innovation.
Most importantly, the model was able to identify visually imperceptible cancer from normal-appearing pancreases on prediagnostic CT images (i.e., those acquired at three to 36 months prior to clinical diagnosis) substantially early — a median of 438 days — before clinical diagnosis.
Dr. Goenka added, “These findings suggest that AI has the potential to detect hidden cancers in asymptomatic individuals, allowing for surgical treatment at a stage when a cure is still achievable.”
Finally, the model remained consistent and accurate over a wide range of patient groups and scanning equipment and imaging methodologies. This robustness is critical for the model’s applicability in a wide range of real-world medical circumstances.
Addressing a fundamental problem in the AI healthcare scene, the team also dissected the AI’s decision-making process to ensure openness and understanding that trust and quality control are critical for AI’s broader clinical acceptability.
Dr. Goenka noted, “We owe the progress to the ingenious efforts of the Framework for AI Software Technology, or FAST, team led by Panagiotis Korfiatis, Ph.D., complemented by our team of exceptionally bright research fellows and data science analysts. They dedicated months to meticulous preparation for our initial submission and invested significant effort to astutely address the incisive queries of the panel of international reviewers.”
He added, “We are only at the beginning but stand ready to address the challenges of early cancer detection, leveraging the capabilities of AI and next-generation molecular imaging in conjunction with complementary biomarkers.”
The Mayo Clinic has already started the clinical validation procedure, and the models are going through regulatory approvals. The team plans to conduct benefactor-funded prospective screening trials with the help of the Mayo Clinic Comprehensive Cancer Center. These studies’ findings will help to refine and improve the practical efficacy of their revolutionary strategy.
Their multidisciplinary effort includes co-authors from Radiology (Garima Suman, MD, Nandakumar Patnam Gopal Chetty, MBBS, MD, Kamaxi H. Trivedi, MBBS, MD, Aashna M. Karbhari, MBBS, MD, Sovanlal Mukherjee, Ph.D., Cole J. Cook, Ph.D., MS, Jason R. Klug, Ph.D., Naveen Rajamohan, MD, Hala A. Khasawneh, Joel G. Fletcher, MD, Candice W. Bolan, MD, and Kumar Sandrasegaran, M.B., Ch.B.), Surgery (Mark J. Truty, MD, MS), and Gastroenterology (Shounak Majumder, MD, Suresh T. Chari, MD).
The research was funded by the National Cancer Institute of the National Institutes of Health under grant numbers R01CA272628 and R01CA256969, as well as the Centene Charitable Foundation and the Funk Zitiello Foundation’s Champions for Hope Pancreatic Cancer Research Program. The authors are entirely responsible for the material, which does not necessarily represent the official views of the National Institutes of Health.