Reviewed by Alex SmithApr 6 2022
According to a new study published in the journal Radiology, researchers were able to detect early symptoms of type 2 diabetes on abdominal CT scans using a completely automated AI deep learning technique.
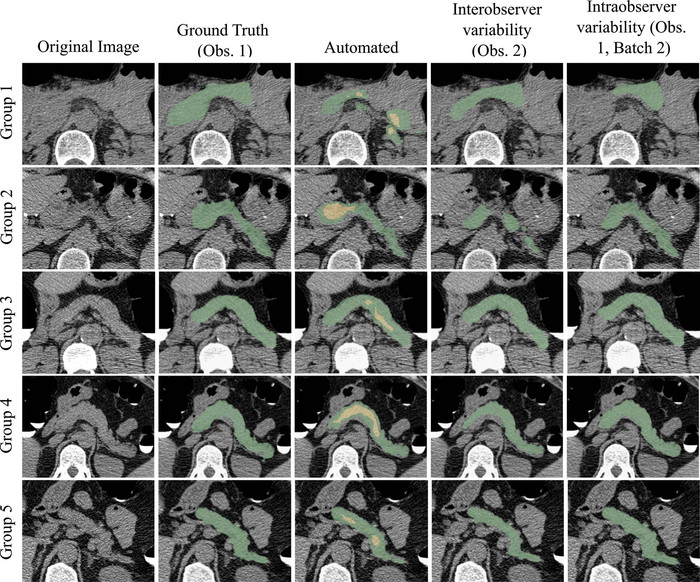
Pancreas segmentation in patients from each of the five visceral fat groups. Segmentation performance is better for patients with higher visceral fat (group 5 being the highest). Visceral fat percentages at the L1 level for the specific patients shown here were 9.81% in group 1, 13.72% in group 2, 20.19% in group 3, 27.88% in group 4, and 32.42% in group 5; Dice similarity coefficients were 0.36, 0.62, 0.78, 0.81, and 0.86, respectively. In the automated segmentation images, the green area indicates full segmentation and the yellow area indicates segmentation after erosion. Obs. = observer. Tallam et al, Radiology 2022; 000:1-11. Image Credit: Radiological Society of North America 2022.
Approximately 13% of all individuals in the United States have type 2 diabetes, while another 34.5% of persons have prediabetes. Due to the disease’s gradual onset of symptoms, it is critical to treat it early. Prediabetes can persist for up to eight years in certain situations, and an earlier diagnosis allows patients to undertake lifestyle adjustments to slow the disease’s progression.
Abdominal CT imaging has the potential to be a useful technique in the diagnosis of type 2 diabetes. CT imaging is already used in clinical practice, and it may reveal a lot about the pancreas.
Diabetes patients acquire more visceral fat and fat inside the pancreas than non-diabetic persons, according to previous research. According to co-lead author Ronald M. Summers, MD, Ph.D., senior scientist and staff radiologist at the National Institutes of Health Clinical Center in Bethesda, MD, however, not much work has been done to analyze the liver, muscles and blood arteries around the pancreas.
The analysis of both pancreatic and extra-pancreatic features is a novel approach and has not been shown in previous work to our knowledge.
Hima Tallam, MD, Study First Author and PhD Student, Department of Radiology and Imaging Sciences, National Institutes of Health Clinical Center
A radiologist or trained expert must manually analyze low-dose non-contrast pancreatic CT images, which is a time-consuming and complex task. According to the authors, there is a need to enhance automated pancreatic image processing to meet these clinical problems.
Diabetic Patients Had Lower Pancreas Density and Higher Visceral Fat
Dr. Summers and colleagues used a dataset of patients who had undergone routine colorectal cancer screening with CT at the University of Wisconsin Hospital and Clinics, in close partnership with co-senior author Perry J. Pickhardt, MD, professor of radiology at the University of Wisconsin School of Medicine & Public Health.
Between 2004 and 2016, 572 people were diagnosed with type 2 diabetes, while 1,880 were diagnosed with dysglycemia, which relates to blood sugar levels that are too low or too high, out of 8,992 patients screened. There was no overlap between the diagnoses of diabetes and dysglycemia.
The researchers utilized 471 images from a range of datasets, including the Medical Data Decathlon, The Cancer Imaging Archive, and the Beyond Cranial Vault competition, to develop the deep learning model. After that, the 471 images were separated into three groups: 424 for training, 8 for validation, and 39 for test sets. Results from four rounds of active learning were also included in the study.
The deep learning model produced outstanding results, with little difference between it and manual analysis. The model examined the visceral fat, density and volume of the surrounding abdominal muscles and organs in addition to the numerous pancreatic properties.
Patients with diabetes had a lower pancreatic density and more visceral fat than those without diabetes, according to the findings.
We found that diabetes was associated with the amount of fat within the pancreas and inside the patients’ abdomens. The more fat in those two locations, the more likely the patients were to have diabetes for a longer period of time.
Dr. Summers, Professor, Radiology, University of Wisconsin School of Medicine & Public Health
Intrapancreatic fat percentage, plaque severity between the L1-L4 vertebra level, average liver CT attenuation, pancreas fractal dimension and BMI were the greatest predictors of type 2 diabetes in the final model. These predictions were employed by the deep learning model to accurately distinguish between diabetic and non-diabetic individuals.
“This study is a step towards the wider use of automated methods to address clinical challenges. It may also inform future work investigating the reason for pancreatic changes that occur in patients with diabetes,” the authors concluded.
Journal Reference:
Tallam, H., et al. (2022) Fully Automated Abdominal CT Biomarkers for Type 2 Diabetes Using Deep Learning. Radiology. doi.org/10.1148/radiol.211914.