Researchers at the University of Groningen have taught an AI system to recognize a certain pattern in skin biopsies from patients with epidermolysis bullosa acquisita, a blistering disease.
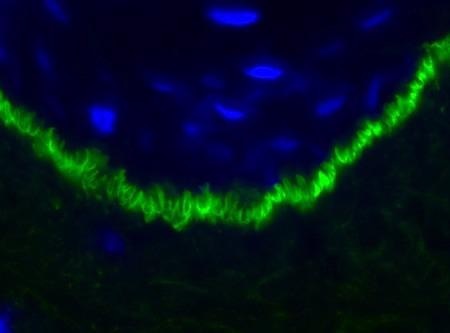 The U-shaped pattern (in green) visible in the skin biopsy of an EBA patient. Image Credit: UMCG/UoG.
The U-shaped pattern (in green) visible in the skin biopsy of an EBA patient. Image Credit: UMCG/UoG.
The pattern is specific to a type of disease that can result in scarring of the skin and mucous membranes, as well as blindness. The new method is simple to use and makes better diagnoses than most doctors. The American Journal of Pathology provides a description of this AI system.
Layers of the skin detach in patients with epidermolysis bullosa, resulting in huge blisters. Blister infections can affect different layers of the skin in different ways. Epidermolysis bullosa acquisita (EBA), for example, is an autoimmune condition in which a patient’s own antibodies assault his or her skin.
It typically begins in middle age, and the blisters might leave scars. Scarring on the skin can limit joint movement but scarring in the mucous membranes can also occur. This can result in blindness if it happens in the eye, for example. Scarring can be avoided with early detection and treatment.
Pattern
At the moment, it can take months to years before the diagnosis of EBA is confirmed.
Joost Meijer, Study Co-First Author and Dermatologist, University Medical Center Groningen
EBA is diagnosed via skin biopsies in which fluorescent markers bind to autoantibodies in the basal layer of the epidermis. This results in a characteristic EBA serrated U-shaped pattern.
However, you need to find and recognize this pattern in a relatively large, microscopic slide.
Joost Meijer, Study Co-First Author and Dermatologist, University Medical Center Groningen
The pattern might only be seen in a few spots on the slide. To give an idea of how small it is, the pattern could only take up 30 × 30 pixels if the microscopic image is digitized as a photograph with a resolution of 20,000 x 12,000 pixels.
Meijer’s Master’s thesis focused on diagnosing strategies for detecting this trend. He subsequently went on to examine the subject as part of his PhD research at the University of Groningen’s Bernoulli Institute for Mathematics, Computer Science, and Artificial Intelligence, where he collaborated with fellow PhD student Astone Shi.
Shi, the paper’s other co-first author, works with Convoluted Neural Networks (CNNs), a sort of deep learning system that is particularly well suited for pattern recognition.
Patients
One challenge was that there is no standard training program for this particular pattern.
Astone Shi, Bernoulli Institute for Mathematics, Computer Science and Artificial Intelligence, University of Groningen
He needed to figure out what kind of CNN to use and how to train it. “There are millions of parameters in these neural networks, and we had to find the ones that work best,” added Shi.
Another issue is obtaining data to train the CNN with. People with EBA are uncommon; in the Netherlands, only about 5 to 10 patients are diagnosed each year. Biopsies from 46 patients were used by Meijer and Shi; 42 were used to train the networks, while the remaining four were used to validate the system.
The AI system was able to distinguish EBA with 89.3% specificity and sensitivity after training nine different CNNs and repeating the method 10 times. This is higher than the accuracy of a small group of highly trained professionals and lower than the accuracy of a group of pathologists and dermatologists.
“This means that our system outperforms most doctors. The reason for this is probably that the human eye only takes a relatively small portion of a microscopic slide into account,” noted Shi.
“Observers get a first impression from this, and then search the slide for confirmation. The AI system analyses the entire slide, which results in a more accurate diagnosis,” stated Meijer.
European study
The key benefit of this digital system is that it is simple to operate. “We envisage a system where you upload an image and then get a diagnosis from the AI algorithm,” stated Meijer.
It might, however, be used to teach clinicians how to recognize the EBA’s particular U-serrated pattern. Although the algorithm performed admirably in this study, the results must be validated using a new, larger dataset. A prospective European study has been launched for this goal.
“It will take a year to collect the data of new skin biopsies, which will be able to validate the system. Hopefully, we will then have a quicker and easier way to diagnose EBA and prevent the sometimes debilitating scarring,” concluded Meijer.
Journal Reference:
Shi, C., et al. (2021) Use of convolutional neural networks for the detection of u-serrated patterns in direct immunofluorescence images to facilitate the diagnosis of epidermolysis bullosa acquisita. American Journal of Pathology. doi.org/10.1016/j.ajpath.2021.05.024.